By Stephen Bunting, Specialist MSK Physiotherapist (UK)
This article is about thumb base osteoarthritis (OA). The main aim to is to provide information and advice about the condition with an emphasis on self-help. The information is also provided in video format below.
The article is written on the assumption that the reader has been diagnosed with thumb base OA by a health care professional. If you haven't been diagnosed but you think you might have the condition then its best to get checked out first as there are other conditions that can cause similar symptoms.
The article address thumb base OA by answering the 3 most common questions that people ask after they have been diagnosed.
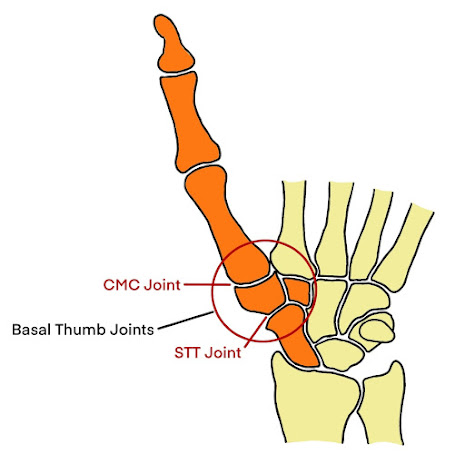
1) What is Thumb Base Osteoarthritis ?
 |  |
 |  |  |
 |
| Repetitive Pinch Gripping |
3) What can I do about it ?
If you've read my article about generalised OA you will have seen how important regular exercise is in helping the condition. But while the evidence strongly supports the use of regular exercise for most arthritic joints, it is less convincing when it comes to exercises for thumb base OA.
This may be because the thumb is such an active joint in most people that it rarely needs additional exercise. But if you do try exercise as a first line treatment then in my experience its best to use movements that don't compress and rotate the thumb at the same time. So avoid strong pinch gripping or other strenuous movements, which will usually be the type of activities that aggravate the symptoms anyway. Instead do regular simple movements to help with joint stiffness such as thumb to finger tapping but try to keep them pain free.
 |
| Simple Thumb Exercises |
Thumb Splints
What does help for most people with the condition is some form of splint to help support the joint when doing those activities that cause pain. The idea of a splint is to support the joint while still allowing some movement and hand function.
Some splints will provide minimal support but still allow a lot of movement and others will provide lots of support but not allow much movement at all, and what works best for you will be the splint that provides enough support to help reduce the pain while still allowing enough thumb movement so can still use you hand for things you need to do.
Splint 1
 |
| Fabric Thumb Splint - Click on Picture for Link |
This first splint is a good starting point as it is inexpensive and provides a decent amount of support while still allowing a good range of thumb movement. It's made of fabric, but with a supportive bar that runs along the thumb. It's secured with a Velcro strap around the wrist and another one around the thumb tip. It comes in different sizes depending on your wrist circumference.
The splint below is very similar but more hard wearing and therefore recommended for longer term use.
 |
| Fabric Splint 2 - Amazon Link |
Splint 2
 |
| Ligaflex Thumb Splint - Click on Picture for Link |
If your arthritis is more severe or you need a splint with more support then the next one I can recommend will do just that but it will restrict your thumb movement a bit more. This one is again made mainly of fabric but it has a plastic wedge that sits between the thumb and index finger. It's secured with a wrist strap and thumb tip strap. It’s a bit more compact than the last one and also more hard wearing.
Splint 3
 |
| Push CMC Thumb Splint - Click on Picture for Link |
The Push CMC Thumb Splint is probably the best splint that you can currently buy as an off-the-shelf thumb base splint but it is quite a bit more expensive than the others. It also very sleek and compact. It was developed by hand therapists and I think it offers the best overall compromise of support and function. So if you want the best available splint that I’ve seen over the years, then this is it. It has a firm plastic piece that neatly surrounds the whole thumb base region and it secures with 2 wrist straps. 3 sizes are available depending on your hand span measurement. It’s quite compact and it doesn’t interfere with wrist movement. It supports the thumb base joints very well while still allowing a good degree of overall hand movement.
Splint 4
All the previous splints are all off-the shelf, and so if your thumb isn’t the typical shape then they might not fit you comfortably and they might cause some pressure. This can particularly happen if your arthritis is late stage and you’ve developed a degree of thumb base squaring. In this case the angled edge of the thumb can rub against the splint and become uncomfortable.
So if this is you, and you can’t find a splint to fit then I would consider my last recommendation, which is a bespoke custom made splint that is moulded to the individual shape of your thumb. These are usually made of a thermoplastic which becomes malleable in hot water so it can be moulded, and when it cools it hardens and retains its shape.
 |
| Custom Made Thumb Splint |
For a custom made splint, you’re going to need to see a Hand Therapist who are usually Occupational Therapists, Physiotherapists or Physical Therapists who have specialised in hand therapy. Some Orthotists will also provide this service.
How to use a Thumb Splint
When you first start wearing a splint you should try to use it for most of the time, even at night if your pain is keeping you awake. The idea is to give your thumb as much rest as possible and allow it to calm down.
About 6 weeks of maximum use is usually needed. Take it off when washing your hands and doing the gentle exercises we mentioned before to prevent stiffness but otherwise, leave it on for the rest of the time.
After about 6 weeks, if its working well, your thumb pain should have improved and you can now start slowly weaning off the splint over a few weeks. During this time, one of 2 things will happen.
1) You might be lucky and the thumb pain might have settled down and as long you can avoid those strenuous activities that aggravated it in the first place, it might stay pain free.
2) Your thumb pain might return as you start reducing the splint use. If that happens then you might need to continue using the splint for the long term but use it just as much as you need to in order to keep the symptoms at bay. You will have discovered the right amount for you during the weaning process.
Medication
Simple pain killers and anti-inflammatories can also be helpful for thumb OA. A short course of anti-inflammatory tablets such as ibuprofen can help to settle a painful flare up. Anti-inflammatory gel can also be effective and can be used in the longer term. Always speak to pharmacist or prescribing clinician before using anti-inflammatories as not everyone can take them.
Recent studies have also found that using a cream derived from Chilli peppers, called capsaicin cream can help with arthritic joint pain when used regularly. In the UK, this is a prescription only medicine and so you will need to see a prescribing clinician.Other Treatment Options
If your thumb pain still persists despite the use of exercises, splints and by modifying your actives then you may need to talk to a health care professional about other options, including injections and surgery.
A cortisone injection can be an effective treatment to settle pain and swelling but they should be done sparingly as cortisone can be harmful if used too much.Other injections that can be considered are the visco-supplementation injections, based on a hyaluronic acid, PRP injections and stem cell injections. These are specialised injections usually done under image guidance and you would need to consult a specialist hand clinician.
Finally, if you're still struggling with thumb pain that is significantly affecting your quality of life then you might need to talk to hand surgeon. There are a number of different procedures available to help with thumb base OA, depending on the particular joints involved, your age and the type of activities you are expecting to do.
__________________________________________________________________________
This article provides general information related to various medical conditions and their treatment. It is intended for informational purposes only. It is not a substitute for professional advice, diagnosis or treatment provided by a doctor or other qualified health care professional. The information provided does not constitute personal advice or guarantee of outcome and should not be used to diagnose yourself or others. You should never ignore advice provided by a health care professional because of something you have seen or read on this website. You should always consult a doctor or other qualified health care professional for personal medical advice.




