Pisotriquetral Joint Pain: A Rare but Often Missed Cause of Wrist Pain
Wrist pain is common — but some causes are so rare that they often go undiagnosed. If you’re experiencing pain and sometimes a grinding or clicking sensation on the palm side of your wrist, just over a small bony bump on the little finger side, you might be one of the few people affected by pisotriquetral joint pain.
So, what exactly is the pisotriquetral joint? And what can go wrong with it? Let’s take a closer look.
You can also see this information in video format below.
What Is the Pisotriquetral Joint?
The pisotriquetral joint is formed by two of the eight small bones in the wrist: the pisiform and the triquetral. These bones sit on the ulnar side (the little finger side) of your wrist. The pisiform is a small, pea-shaped bone (its name actually comes from the Latin word pisum, meaning “pea”) that you can feel on the palm side of your wrist — it feels like a small marble under the skin.
The pisiform rests against the triquetral bone, forming the pisotriquetral joint — a small but important connection in wrist mechanics.
What Does This Joint Do?
The pisiform serves as the attachment point for a key muscle: the flexor carpi ulnaris (FCU). This muscle helps flex your wrist and its tendon uses the pisiform as a fulcrum — a bit like the kneecap works for your thigh muscles. By re-angling the tendon’s pull, the pisiform helps your wrist to flex more efficiently.
 |
What Can Go Wrong With It?
There are two main problems that can affect the pisotriquetral joint:
1. Osteoarthritis (Wear and Tear)
Just like any other synovial joint, the cartilage surface between the pisiform and triquetral bones can wear down over time. This leads to osteoarthritis, where the joint surfaces become rough and painful. People often describe a grating or grinding sensation with wrist movement.
2. Instability (Ligament Injury)
Sometimes, after an injury such as a fall, the ligaments holding the pisiform in place can be torn or overstretched. This causes the pisiform to become unstable, wobbling around under the pull of the FCU tendon. This instability can feel like something’s shifting or clicking in your wrist and, if left untreated, can eventually lead to arthritis.
What Are the Symptoms?
People with pisotriquetral joint problems often report:
-
Localised pain on the palm side of the wrist
-
Discomfort when flexing the wrist or leaning on the hand (e.g. doing push-ups or getting up from a chair)
-
A feeling of movement or instability in the wrist
-
Occasionally a grinding or popping sensation
How Is It Diagnosed?
🧪 Clinical Testing – The Pisotriquetral Grind Test
This is a hands-on test carried out by a clinician:
-
The pisiform is pinched between the thumb and finger.
-
The wrist is flexed to relax the FCU tendon.
-
The pisiform is gently moved side-to-side and pressed down toward the triquetral.
-
Reproduction of pain or a grinding sensation is considered a positive test.
-
It’s often compared to the other wrist to assess instability.
🖼️ Imaging
-
X-ray is often used to identify osteoarthritis, showing rough or worn joint surfaces.
-
If instability is suspected, an MRI or MR arthrogram is more useful, as it can show the condition of the supporting ligaments.
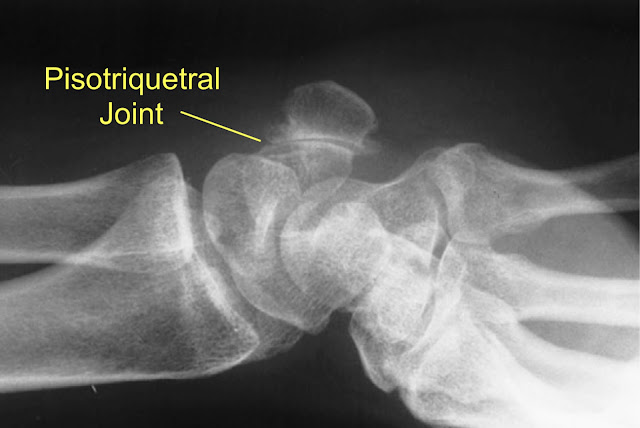
An X-Ray showing Arthritis of the Pisotriquetral Joint
How Is It Treated?
🩹 For Acute Injury or Instability
-
Immobilisation in a wrist splint for 6 weeks allows ligaments to heal.
-
More severe injuries may require a cast and orthopaedic care.
-
Anti-inflammatory medication (tablets or gel) can help ease pain.
💊 For Osteoarthritis
-
Splints and anti-inflammatories can settle flare-ups.
-
Avoiding aggravating activities (e.g. racket sports, painting, heavy wrist use) is often helpful.
💉 Corticosteroid Injection
-
If symptoms persist, a steroid injection into the joint can significantly reduce inflammation and pain.
-
For some, this may be a long-term solution or even a permanent fix — especially if you avoid repeat aggravation.
🛠️ Surgical Options
-
If pain remains problematic despite other treatments, surgery may be an option.
-
The most common procedure is a pisiform excision (removal of the bone).
-
Most people do very well afterward — wrist flexion strength may reduce slightly, but the pain relief is often worth it.
You can watch a pisiform excision here, but be aware that this video shows a real operation.
Summary: Should You Be Concerned?
Pisotriquetral joint pain is rare but real — and it’s often missed or misdiagnosed. If you’ve had ongoing wrist pain on the ulnar side of your wrist, particularly with flexion or pressure, and especially after a fall or injury, this could be the root of the issue.
The good news? Once diagnosed, it’s usually very treatable — often with splinting or injection, and occasionally with surgery.
Need Support?
If you think this might be your problem, speak to a physiotherapist or GP with experience in wrist conditions. Early diagnosis can save months (or years) of confusion and discomfort.
_____________________________________________________________________________
This article provides general information related to various medical conditions and their treatment. It is intended for informational purposes only and not a substitute for professional advice, diagnosis or treatment provided by a doctor or other qualified health care professional. The information provided does not constitute personal advice or guarantee of outcome and should not be used to diagnose yourself or others. You should never ignore advice provided by a health care professional because of something you have seen or read on this website. You should always consult a doctor or other qualified health care professional for personal medical advice.





















